Closing the Coverage Gaps: Reducing Health Insurance Disparities in Massachusetts
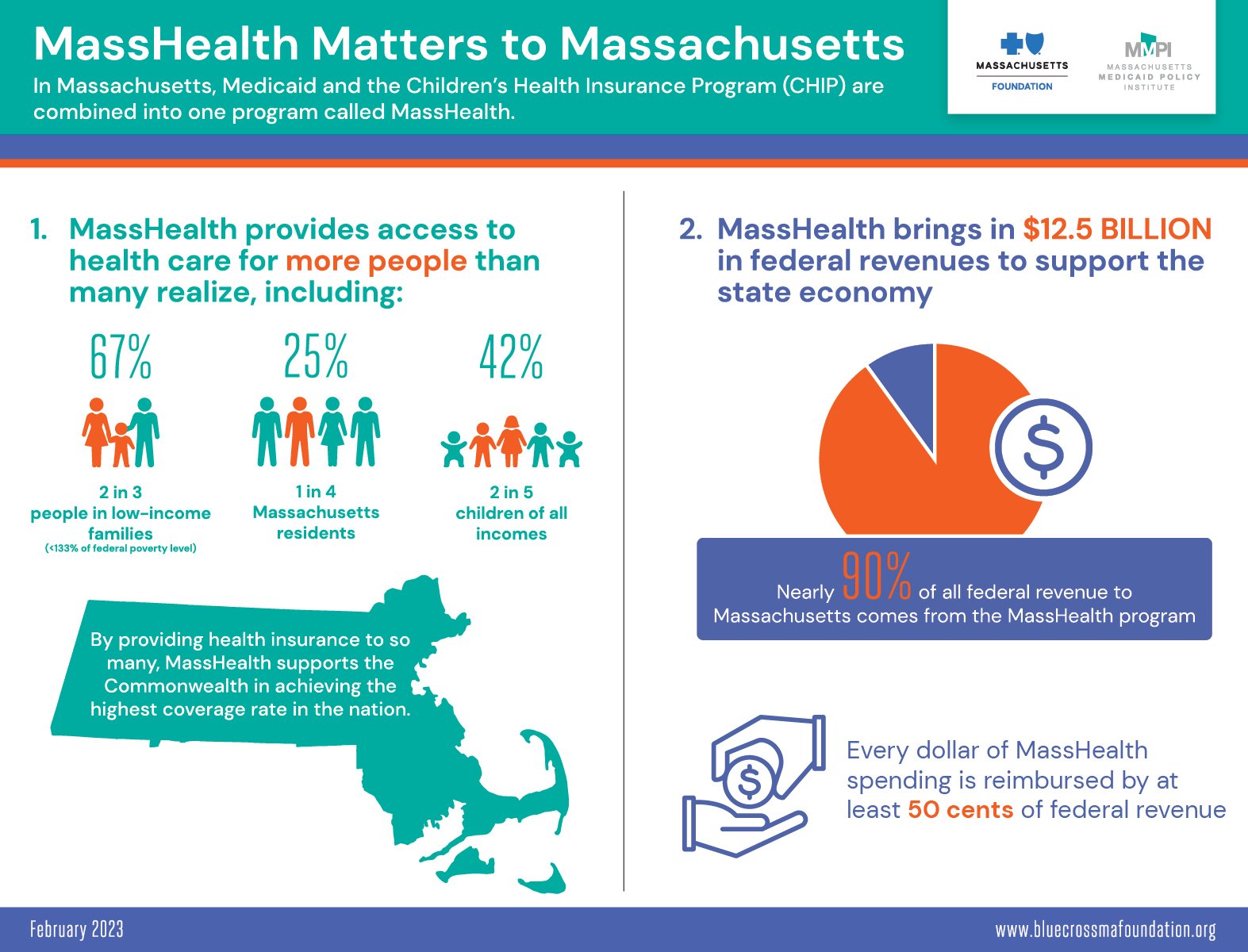
Massachusetts has been exemplary in developing health insurance coverage policies to cover its residents. By 2019, the state’s uninsurance rate was 3.0 percent, the lowest rate in the nation, representing about 204,000 uninsured residents. While the state’s overall uninsured rate at a given point in time is low, more than twice as many people - 503,000, or 7.3 percent of the population - experienced a gap in coverage over the previous twelve months. And importantly, not all groups benefit equally. People who are Black or Hispanic, or who have lower incomes, experience significantly higher rates of uninsurance than the state population overall. As a result, these groups are more likely to face access barriers and financial insecurity associated with being uninsured.
The purpose of this report is to begin charting a course toward closing the coverage gaps in Massachusetts, with a particular focus on creating a more racially and ethnically equitable system of coverage. The report and accompanying infographics describe the people in Massachusetts without health insurance and the barriers to coverage they face, including affordability, administrative complexity, and immigration, language, and cultural barriers. It then proposes a menu of policy options that address the specific circumstances in Massachusetts. The proposed options are meant to inform a statewide conversation about the best approaches to closing the remaining coverage gaps in Massachusetts and removing structural barriers that result in racial and ethnic disparities in health insurance coverage.
Behind the Data: Voices of the Uninsured
The Foundation recently released a 3-minute video featuring four Massachusetts residents who describe their experiences without health insurance. The video is also available with English subtitles and Spanish subtitles (con subtitulos en Español).