The Blue Cross Blue Shield of Massachusetts Foundation today announced that thirteen health and science journalists from across the nation have been selected for the 2023 class of the Health Coverage Fellowship.
The 2023 fellows are Jessica Bartlett of the Boston Globe, Selena Simmons-Duffin of NPR, Sara Willa Ernst of Houston Public Media, Sruthi Gopalakrishnan of the Concord (NH) Monitor, Mark Herz of Boston’s GBH, Keren Landman of Vox, Deidre McPhillips of CNN, Alaa Mostafa of PRX’s This American Life, David Ovalle of the Washington Post, Emily Wagster Pettus of the Associated Press in Mississippi, Laura Santhanam of PBS NewsHour, Sujata Srinivasan of WNPR in Connecticut, and Sarah Toy of the Wall Street Journal.
The fellowship is designed to help the media improve its coverage of critical health care issues. It does that by bringing in as speakers more than 75 health officials, practitioners, researchers, and patients. It also brings the journalists out to watch first-hand how the system works, from walking the streets at night with mental health case workers to visiting the world’s biggest brain bank.
The program, which is entering its twenty-second year, is sponsored by the Blue Cross Blue Shield of Massachusetts Foundation, with support from the Bower Foundation in Mississippi, Commonwealth Fund, Connecticut Health Foundation, Endowment for Health in New Hampshire, Fledgling Fund, National Institute for Health Care Management Foundation, Rita Allen Foundation, Robert Wood Johnson Foundation, and, in Texas, the Episcopal Health Foundation, Meadows Mental Health Policy Institute, Methodist Healthcare Ministries, and St. David’s Foundation.
The fellowship will run for nine days, beginning September 29, 2023. It is housed at Babson College’s Executive Conference Center in Wellesley, MA. Larry Tye, who covered health and environmental issues at the Boston Globe for 15 years, directs the program. A former Nieman Fellow and author of nine books, Tye has taught journalism at Boston University, Northeastern, Tufts, and Harvard.
Next fall’s fellowship will focus on a series of pressing issues – from preventing future pandemics to treating mental illness, rooting out racial and ethnic inequities, redressing homelessness, and rethinking later-life care. Attention also will be given to breakthroughs in medical treatments and curbing health-care costs.
The teaching will not end when fellows head back to their outlets. Tye, the program director, will be on call for the journalists for the full year following their nine days in Wellesley. He will help when they are stuck for ideas or whom to call on a story. He also will assist in thinking out projects and carving out clearer definitions of beats.
About the Blue Cross Blue Shield of Massachusetts Foundation
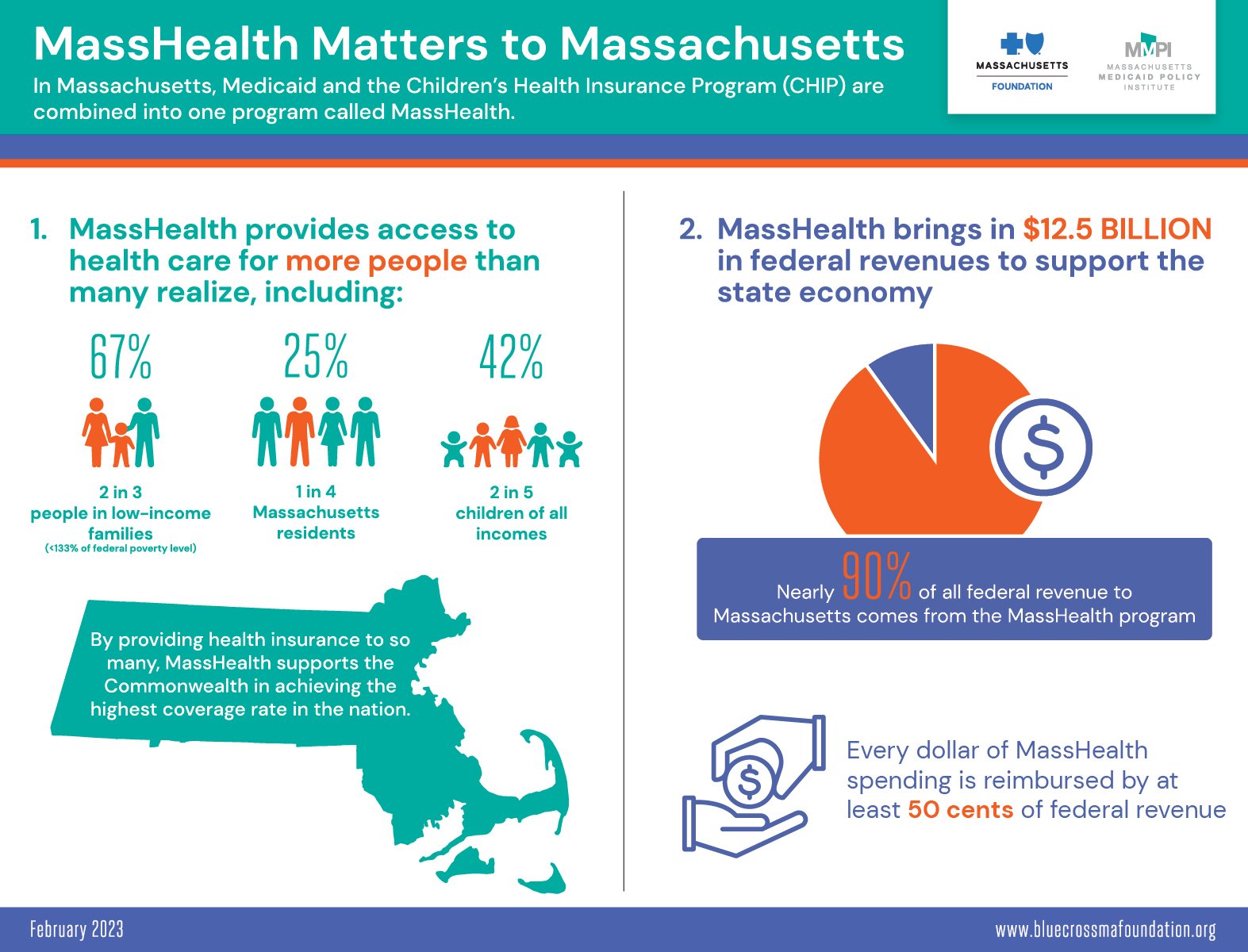
The mission of the Blue Cross Blue Shield of Massachusetts Foundation is to ensure equitable access to health care for all those in the Commonwealth who are economically, racially, culturally or socially marginalized. The Foundation was established in 2001 with an initial endowment from Blue Cross Blue Shield of Massachusetts. It operates separately from the company and is governed by its own Board of Directors. More information is available at www.bluecrossmafoundation.org.