What is the Actual State Cost of MassHealth in State Fiscal Year 2022?
As a program that provides publicly-funded health benefits to more than 2 million low-income children and families, seniors and people living with disabilities in Massachusetts, it is not surprising that MassHealth accounts for a large share of the state’s budget. However, a cursory review of the MassHealth budget can be misleading because it can obscure the billions of dollars in federal revenue that the program generates for the state. This brief looks beyond the budget totals to help stakeholders better understand the actual state cost of MassHealth by accounting for the state and federal partnership that finances this program.
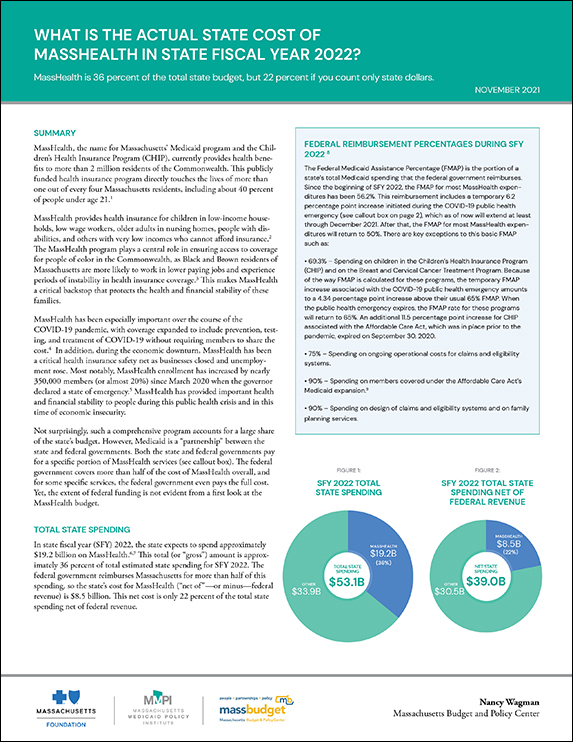
In state fiscal year (SFY) 2022, the state projects it will spend approximately $19.2 billion on MassHealth. This total (or “gross” amount) is approximately 36 percent of total estimated state spending for SFY 2022. However, because the federal government reimburses Massachusetts for more than half of its MassHealth spending, the state’s actual cost for MassHealth (“net of”—or minus—federal revenue) is $8.5 billion or 22 percent of the total state spending in SFY 2022. Fully understanding the actual state cost of MassHealth requires appreciating the details of the federal and other revenue sources that support this essential and comprehensive program.