Philanthropy and Health Reform, 1982-2008
Community Catalyst report on the role that foundations and other philanthropic organizations played during more than two decades of health care reform efforts in Massachusetts. (January 2009)
Community Catalyst report on the role that foundations and other philanthropic organizations played during more than two decades of health care reform efforts in Massachusetts. (January 2009)

On December 22, 2008, the Centers for Medicare and Medicaid Services approved Massachusetts' request to renew the MassHealth Section 1115 Research and Demonstration Waiver (Waiver) for an additional three years, through the end of state fiscal year 2011. The Waiver, which has been in place since 1997, authorizes critical federal funding for several health coverage programs for low-income individuals and for the Commonwealth's safety net health system for uninsured residents. It is the programmatic and financial underpinning of the state's health care reform law. Through the Waiver, over 1 million low-income children, families and individuals receive coverage through MassHealth and Commonwealth Care, the subsidized premium assistance program for low-income adults created by Chapter 58. This report explains how the state's Waiver works.

This report is the first assessment of how spending to insure hundreds of thousands of additional people in the Commonwealth is being shared. It finds that the overall distribution of spending on health insurance by employers, individuals, and government remained essentially the same between 2005, one year before passage of the 2006 Massachusetts health reform law, and 2007, one year into the laws implementation.

This policy brief by Sharon Long of The Urban Institute measures geographic and racial disparities in access to health care in Massachusetts. The data in the brief comes from the third annual Massachusetts Health Reform Survey. This revised version of the policy brief, which was originally published 5/28/2009, reflects changes made after an error in constructing survey weights was discovered and corrected. These changes do not impact the basic findings and conclusions in the original policy brief with respect to geographic differences; however, it does lead to more evidence of racial/ethnic differences in the affordability of health care in Massachusetts.

This policy brief describes the rate of uninsurance among working-age adults in Massachusetts and public support for health reform. This brief is part of a series funded by Blue Cross Blue Shield of Massachusetts Foundation, the Commonwealth Fund, and the Robert Wood Johnson Foundation on implementation of the Massachusetts reforms.

This policy brief based on data from the 2008 Massachusetts Health Reform Survey shows that while health reform in Massachusetts has succeeded in increasing health insurance coverage and access to care, use of emergency departments by working-age residents remains high. Those seeking care in EDs 5/have trouble accessing care in other settings. They are less likely to use a doctors office or private clinic as their usual source of care and they are somewhat less likely to report having a place they usually go to (other than the ED) when they are sick or need advice about their health. And frequent users of emergency rooms (those reporting more than three ED visits in a year) are a sicker, more disabled and chronically ill population than other adults in the state.
This analysis outlines the potential impact a national health reform bill may have on Massachusetts, including key areas that bear further monitoring.
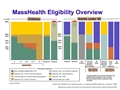
MassHealth eligibility has expanded through a series of incremental steps since 1997. This chart shows the populations that have been made eligible for MassHealth as a result of these expansions, by category and income level (relative to the federal poverty guidelines).

This report is based on a survey of 1,982 mental health providers in Massachusetts including psychiatrists, psychiatric clinical nurse specialists, psychologists, social workers, mental health counselors, and marriage and family therapists. It estimates the need for childrens mental health services; assesses child and family mental health service delivery capacity; identifies variation in capacity, including variation by geography, linguistic ability, and cultural competence; and documents challenges to meeting current demand for services.

On November 13, 2009, MMPI partnered with the Massachusetts Health Policy Forum and Community Catalyst to sponsor a forum exploring efforts in Massachusetts to improve quality and control Medicaid prescription drug costs. At the forum, an issue brief was released that detailed implementation of a preferred drug list in the MassHealth program. In addition, speakers talked about the array of tools available to states to improve prescribing and reduce cost growth.
Click here to see the agenda and other materials from the meeting.

MassHealth, the Massachusetts Medicaid program, could play a leading role in implementing dramatic changes to the health care payment system. This report outlines how so-called global payments could be used in MassHealth, which provides insurance coverage to roughly 1.2 million people in the state. Global payments have been recommended by both the Special Commission on Health System Payment and the Massachusetts Health Care Quality and Cost Council as a means of reigning in health care cost increases and improving care coordination.

In August 2009, legal immigrants who have been in the United State for fewer than five years lost their eligibility for health insurance coverage under Commonwealth Care. They now receive coverage under the Bridge Program. In December, the BCBSMA Foundation brought together grantees, government officials, advocates, and health insurers for an informal discussion about how and why these changes were made, and how to improve coverage for legal immigrants.

This report, written in conjunction with senior staff at the Center for Health Law and Economics, examines the phenomenon of enrollees cycling on and off state health insurance programs, specifically MassHealth and Commonwealth Care.