National Health Care Reform and Its Impact on Massachusetts
This analysis outlines the potential impact a national health reform bill may have on Massachusetts, including key areas that bear further monitoring.
This analysis outlines the potential impact a national health reform bill may have on Massachusetts, including key areas that bear further monitoring.

Members of the first class of students in the Massachusetts Institute of Community Health Leadership talk about how the program has influenced the way they work.
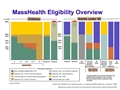
MassHealth eligibility has expanded through a series of incremental steps since 1997. This chart shows the populations that have been made eligible for MassHealth as a result of these expansions, by category and income level (relative to the federal poverty guidelines).

This report is based on a survey of 1,982 mental health providers in Massachusetts including psychiatrists, psychiatric clinical nurse specialists, psychologists, social workers, mental health counselors, and marriage and family therapists. It estimates the need for childrens mental health services; assesses child and family mental health service delivery capacity; identifies variation in capacity, including variation by geography, linguistic ability, and cultural competence; and documents challenges to meeting current demand for services.

On November 13, 2009, MMPI partnered with the Massachusetts Health Policy Forum and Community Catalyst to sponsor a forum exploring efforts in Massachusetts to improve quality and control Medicaid prescription drug costs. At the forum, an issue brief was released that detailed implementation of a preferred drug list in the MassHealth program. In addition, speakers talked about the array of tools available to states to improve prescribing and reduce cost growth.
Click here to see the agenda and other materials from the meeting.

MassHealth, the Massachusetts Medicaid program, could play a leading role in implementing dramatic changes to the health care payment system. This report outlines how so-called global payments could be used in MassHealth, which provides insurance coverage to roughly 1.2 million people in the state. Global payments have been recommended by both the Special Commission on Health System Payment and the Massachusetts Health Care Quality and Cost Council as a means of reigning in health care cost increases and improving care coordination.

December 18, 2009 Lindsey Tucker, the Health Care Policy Manager for Health Care for All, and a graduate of the 2008-2009 Massachusetts Institute for Community Health Leadership, talks about how the program impacted her work, and her colleagues also assess how the program influenced Lindsey.

December 17, 2009 A client in recovery and an employee of Steppingstone Inc., a past grantee in the Connecting Consumers with Care program area, talk about the organization's innovative Project ACCTION program for substance abusers.

December 18, 2009 Members of the 2007 class of the Massachusetts Institute of Community Health Leadership talk about the community created over the nine months of the program. This video should be watched after Anticipating the Road Ahead, which features the same members talking about their expectations for the program.

December 18, 2009 Incoming members of the 2007 class of the Massachusetts Institute of Community Health Leadership talk about what they expect from the program. This video should be watched before Growing A Community, which features the same members talking about their experiences after their completion of the program.

Joe Ianelli, the Financial Services Manager for Massachusetts General Hospital, talks about what he learned as a student of the Massachusetts Institute for Community Health Leadership.

Jennifer Chow, the Grantmaking Program Manager for the BCBSMA Foundation, participated in the Massachusetts Institute of Community Health Leadership in 2006 and 2007, when she was the Outreach and Enrollment Manager for Health Care for All. In this video, she talks about the impact the program has had on her work and how she interacts with grantees.

In August 2009, legal immigrants who have been in the United State for fewer than five years lost their eligibility for health insurance coverage under Commonwealth Care. They now receive coverage under the Bridge Program. In December, the BCBSMA Foundation brought together grantees, government officials, advocates, and health insurers for an informal discussion about how and why these changes were made, and how to improve coverage for legal immigrants.

This report, written in conjunction with senior staff at the Center for Health Law and Economics, examines the phenomenon of enrollees cycling on and off state health insurance programs, specifically MassHealth and Commonwealth Care.

This policy brief based on data from the 2009 Massachusetts Health Reform Survey shows that women have achieved significant gains in insurance coverage and in access and use of health care since health reform was implemented in Massachusetts. The gains were particularly strong for subgroups of women who had lower levels of coverage and poorer access prior to reform, including lower-income women, women of minority race/ethnicity, and women without dependent children.